Abstract
Introduction:
Thrombotic Thrombocytopenic Purpura (TTP) is a hematological emergency with high inpatient mortality that requires prompt diagnosis and treatment. Studies outside the setting of hematologic emergencies have established hospital volume as a factor associated with clinical outcomes. We tested whether hospital volume was associated with important inpatient outcomes among patients with TTP
Methods:
We utilized the Nationwide Inpatient Sample (NIS) to identify adult patients ≥18 years, diagnosed with TTP using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code 446.6 from the years of 2010 to 2013. We only included patients who received therapeutic plasmapheresis (ICD-9-CM procedure code 99.71) during hospitalization to capture active cases of TTP and improve coding accuracy. Using unique hospital identifier, hospital volume was computed and defined as total hospitalizations for TTP per year. Hospital volume was then divided into four quartiles. The primary outcome of interest was inpatient mortality rate, with time to initiation of plasmapheresis as our secondary outcome. Baseline age, gender, race, demographics, insurance payer, hospital region, hospital type (rural versus urban, teaching versus non-teaching), and bed size were collected. All analyses were survey adjusted to account for the complex sampling nature of the database. Appropriate bivariate methods included ANOVA and tests of trend (nptrend). Mixed effects hierarchical logistic regression analysis was used to calculate adjusted odds ratio of in-hospital mortality adjusting for potential confounders at the patient level (age, race, comorbidity, gender, insurance status) and at the hospital level (hospital location, bedsize and teaching status). All p values were two sided and the level of significance was chose was 0.05.
Results:
A total of 1128 unique hospitalizations for TTP were identified during the study period. The mean age was 46.3 ± 16.6 years, out of which 66% were females (n=754) and 44% were whites (n=458). The overall inpatient mortality rate was 10.9%. The distribution of hospital volume by quartiles was as follows; 1st quartile, Q1 (2 or less hospitalizations of TTP per year), 2nd quartile, Q2 (3-5/year), 3rd quartile, Q3, (6-11/year), 4th quartile, Q4 (12 and above). The mean length of stay was 14.4 ± 11.5 days and the mean cost of hospitalization was $ 177546 ± 7736.
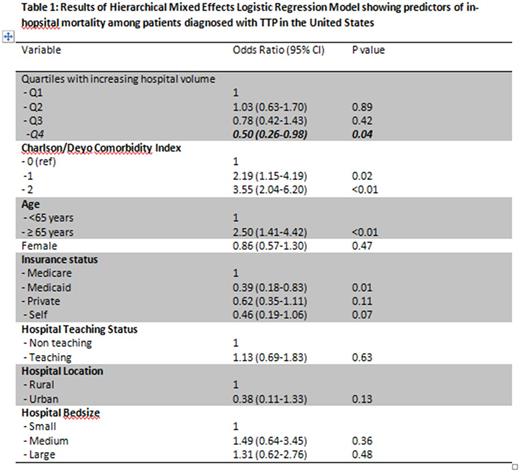
Overall there was decreasing trend in inpatient mortality with increasing hospital volumes (14.4% vs 12.8% vs 9.8% vs 6.5% from Q1-Q4 respectively; p trend 0.002). This effect was also retained in multivariate analysis adjusting for potential confounders (aOR 0.50; 95% CI 0.26-0.98; p 0.04) (Table 1). Also there was a decreasing trend in the time to plasmapheresis with increasing hospital volume (3.02 vs 2.48 vs 2.27 vs 2.09 from Q1-Q4 respectively, ANOVA p value 0.04) with post hoc analysis significant difference between 4th versus 1st quartile (Tukey p value 0.04).
Conclusion:
In this retrospective cohort study using a large US inpatient database, we identified a significant association between hospital volume and inpatient mortality. Furthermore, plasmapheresis was initiated earlier in the hospital course at higher volume hospitals and provides a potential mechanism for the survival improvement.
Podoltsev: Ariad: Consultancy; Incyte: Consultancy; Alexion: Consultancy; CTI biopharma/Baxalta: Consultancy. Huntington: Janssen: Consultancy; Pharmacyclics: Honoraria; Celgene: Consultancy, Other: Travel. Zeidan: AbbVie, Otsuka, Pfizer, Gilead, Celgene, Ariad, Incyte: Consultancy, Honoraria; Takeda: Speakers Bureau; Otsuka: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal